If you are confused about your doctor's bill, you are not alone. Medical billing is so complex these days that even your doctor's staff is often perplexed. In this article I'll try to demystify some of the common billing terms.
Billing 101
Your doctor's charges basically boil down to two things:- What the doctor did (the service), and
- Why he did it (the diagnosis)
For each service he bills, the doctor needs to justify it with the diagnosis which includes symptoms and signs. For instance, he provides an office visit (the service) because you have a sore throat (the diagnosis). If he gives you a joint injection and marks high blood pressure as the diagnosis, the insurance company will deny the claim, because hypertension is not a valid reason to do a joint injection. This seems like a simple concept, but it is not always so intuitive. If you have a bone density test, the diagnosis cannot be osteoporosis (which seems plausible), but it can be a loss of height.
Simply choosing the right visit code is a complex task. No doubt you've been miffed when the doctor has spent 5 minutes with you and charged a high fee. But time is not usually a consideration. The three key components in choosing the level of service are the comprehensiveness of the history and examination, and the complexity of the medical decision-making. See more about E/M coding.
There are rules about what services can be billed together. For instance the doctor cannot charge an office visit and a procedure the same day. If you go to the dermatologist to have skin tags removed, she cannot charge you for both the office visit and the skin tag removal. The only way she could justify that would be if you came in for another purpose, perhaps a rash, and while you were there she took off your skin tags too. But seriously, how often does that happen? She is more likely to schedule a return visit for the skin tag removal.
Sometimes a service is not covered at all. You take your daughter to the doctor for a sports physical, and you end up paying out-of-pocket because your insurance will not cover it. You complain that your insurance provides an annual physical, which seems like the same thing to you. But it is an entirely different service as far as your insurance company is concerned. What you should have done is schedule your child for an annual checkup (if due) and take the form with you. They may charge you for the form, but at least you won't have to pay for the examination. Alternatively, if your child has had the annual checkup recently, your doctor may be willing to complete the form without doing another examination.
Often patients will ask the staff to change the diagnosis so that insurance will pay. This is fine if it was a true diagnosis at the time of service, but they cannot make something up. That's called fraud and abuse.
Medical Coding
Medical coding is necessary so that computers can process the high volume of medical claims. Coding converts your services and diagnoses into a uniform alpha-numeric system that is used across all providers and insurance companies in the U.S. and beyond. You will find these codes listed on your encounter form and billing statements. It may help you decipher your bill if you learn a little about the coding.
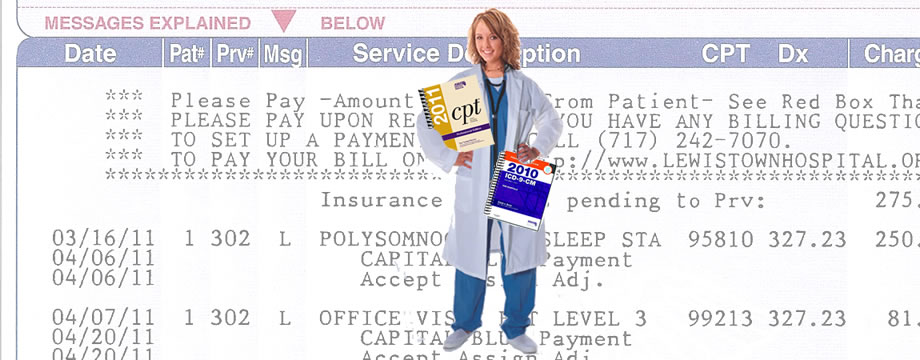
Billing Statement
Service Codes. Most physician service codes come from the American Medical Association's Current Procedural Terminology (CPT). Everything the doctor does, from the office visit to a complicated surgery, has an associated CPT code. Look up service codes on this AMA page. In the example above, my doctor has billed me for two services:
- 95810 - Polysomnography; sleep staging with 4 or more additional parameters of sleep, attended by a technologist, and
- 99213 - Office or other outpatient visit for the evaluation and management of an established patient.
Diagnosis Codes. Dx codes are much more interesting. Perhaps the doctor didn't tell you your diagnosis, but you can look it up yourself. The International Classification of Diseases,Ninth Revision, Clinical Modification (ICD-9-CM) is provided by the National Center for Health Statistics. Here's a free lookup site from Medilexicon. You will be amazed and amused at what you can find in the ICD-9 dictionary. Go ahead and type in any crazy thing you can think of. A fall from a haystack is code E884.9. A legal execution is E978. But you would be more likely to find on your encounter form code 278.0 for overweight or 997.91 for high blood pressure. In the example above, I have the same diagnosis for each service: 327.23 -Obstructive sleep apnea.
In Conclusion
This mini-lesson has only scratched the surface of course. Even as a 21-year medical practice veteran, I still went to our billing manager with my invoice and pleaded, "Mary - just tell me what I owe you." Likewise I recommend that you speak to your doctor's billing staff when you don't understand a charge or think something is amiss. Mistakes do happen in this complicated business, and most billing people truly want to get it right. If you cannot resolve the matter with your doctor's office, go to your insurance company, and if you are still not satisfied, you can file a complaint with your state's insurance department. I guarantee that will get everyone's attention.